Understanding the Health Impacts of Long-Acting Reversible Contraception
Family planning is an essential element of reproductive health and with good reason.
Statista notes that global contraceptive use among women has reached 50% in 2023. However, significant disparities exist across regions. Married women consistently demonstrate higher contraceptive use, reaching 65% globally. The numbers highlight the need for effective and convenient birth control options for all women, regardless of marital status.
Long-acting reversible contraception (LARC) emerges as a solution with its exceptional effectiveness and long-lasting convenience. This article discusses the health impacts of LARC, exploring its potential benefits, side effects, and complications.
Introduction to LARC
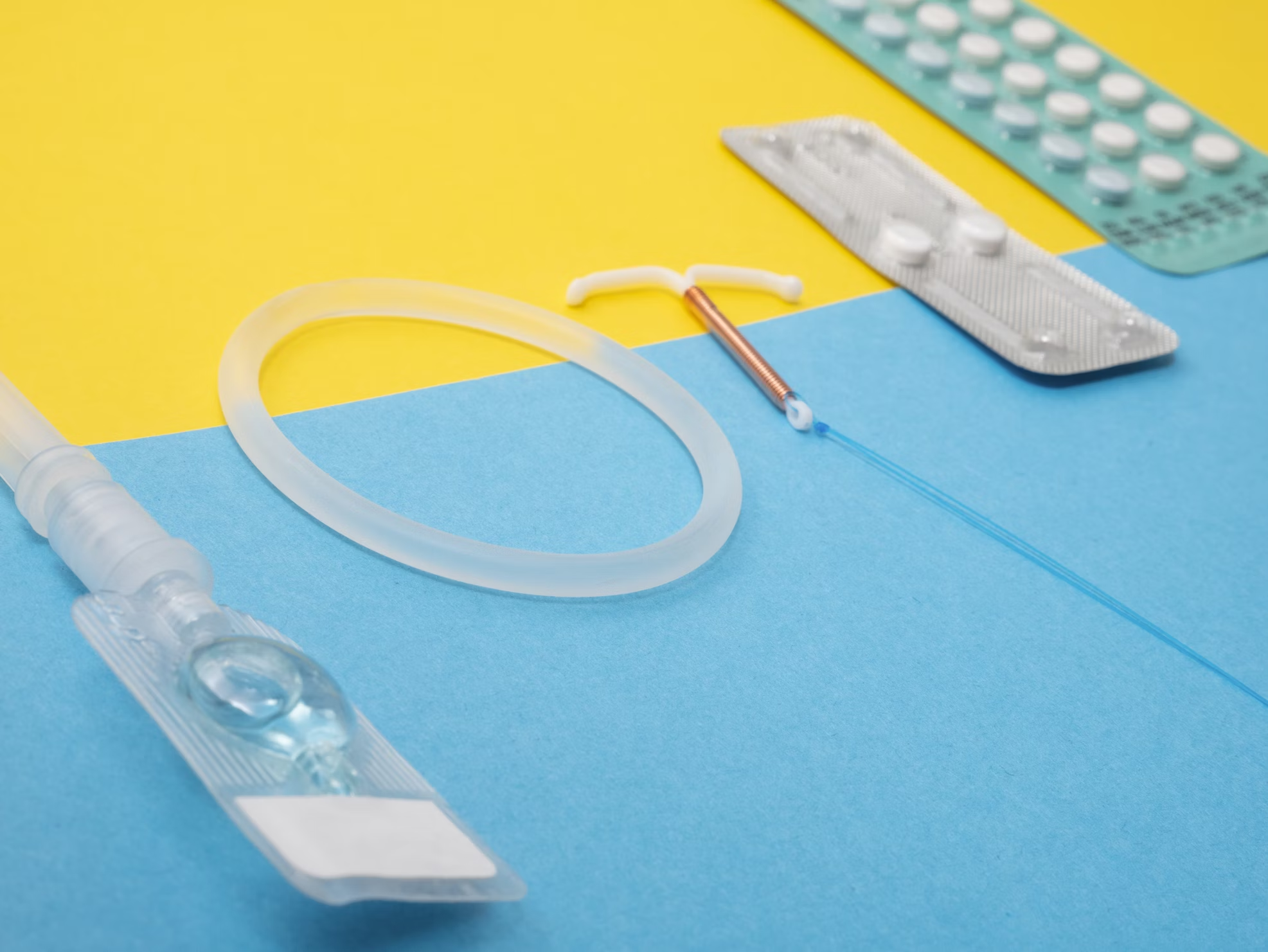
LARC is a highly effective method of birth control that provides long-term pregnancy prevention. According to the Cleveland Clinic, LARCs come in two main forms:
- Intrauterine Devices (IUDs): A healthcare provider inserts these small, T-shaped devices into the uterus. They come in two varieties: copper IUDs (e.g., Paragard), which last ten years, and hormonal IUDs (e.g., Mirena, Liletta), which last 3-7 years depending on the brand.
- Subdermal Implants: A healthcare provider inserts these matchstick-sized rods (e.g., Nexplanon) under the skin of your upper arm. They prevent pregnancy for up to three years.
LARC’s significance lies in its exceptional effectiveness (over 99% typical use) compared to other methods requiring frequent user action. This translates to a significant reduction in unintended pregnancies. With various options available, LARC caters to diverse needs and preferences, making it a crucial tool in modern contraceptive practices.
LARC’s Mechanism of Action
LARC methods, including IUDs and contraceptive implants, work through different mechanisms to prevent pregnancy effectively. JAMA notes that IUDs are T-shaped devices inserted into the uterus, with strings that extend through the cervix.
Ideally, the hormonal IUDs contain levonorgestrel. It’s a hormone that thickens cervical mucus to prevent sperm from reaching the egg and thins the uterine lining to hinder implantation. In some cases, this hormone also suppresses ovulation.
These IUDs are effective for contraception for three to eight years. They are immediately effective if inserted within the first seven days of a menstrual period. Otherwise, additional contraception or abstinence is recommended for seven days.
Non-hormonal IUDs are made of copper and can provide contraception for up to 12 years. The copper acts as a spermicide, disrupting sperm motility and viability. This makes it immediately effective upon insertion without the need for backup contraception.
Contraceptive implants, like Nexplanon, are small plastic rods placed under the skin of the upper arm. They release progestin, which suppresses ovulation, thickens cervical mucus, and thins the uterine lining. The implant is effective immediately when inserted within the first five days of menstruation. If inserted later, additional contraception or abstinence is advised for seven days.
Health Benefits of LARCs
One of the most notable advantages of LARCs is the reduced risk of certain cancers. Hormonal IUDs are associated with a lower risk of endometrial cancer due to the continuous release of progestin, which thins the endometrial lining. Additionally, both hormonal and non-hormonal IUDs may help reduce the risk of ovarian cancer, although the exact mechanism is not fully understood.
Another major benefit of these contraceptives is their ability to regulate menstrual cycles. Hormonal IUDs can lead to lighter periods or even amenorrhea (the absence of menstruation), providing relief for individuals with heavy menstrual bleeding. This regulation of menstrual cycles improves quality of life and decreases the likelihood of anemia caused by excessive blood loss.
LARCs also contribute to a reduced risk of pelvic inflammatory disease (PID). The presence of an IUD can decrease the risk of ascending infections from the lower genital tract, thus protecting against PID.
In response to these benefits, legislative actions are being taken to improve access to these contraceptives. According to WFYI, Indiana Governor Eric Holcomb signed a bill mandating hospitals to offer Medicaid members the option of receiving a subdermal LARC. This option is available during a delivery visit.
The new law, HEA 1426, ensures Medicaid covers the cost of stocking subdermal LARCs, potentially enhancing access and choice for postpartum contraception.
Potential Side Effects
LARCs can have potential side effects. One common issue is bleeding. Users may experience irregular bleeding, spotting, or heavier periods initially, especially with copper IUDs, although these symptoms often diminish over time.
Mood swings and breast tenderness are other potential side effects, similar to those experienced with hormonal birth control pills. These symptoms are generally linked to the body’s adjustment to the hormones released by the device.
The insertion and removal of these contraceptives can also cause minor discomfort or pain. During insertion, some users report cramping or pain, which usually subsides quickly. Removal is typically less uncomfortable but may still cause brief discomfort. Healthcare providers ensure these procedures are as painless as possible and provide guidance on managing any temporary discomfort.
IUD Complications – A Cause for Concern
LARCs, while highly effective, are not without potential complications. IUDs, specifically the copper IUD Paragard, have been the center of recent lawsuits due to serious concerns.
The Paragard lawsuit alleges a design defect in the T-shaped arms of the device, claiming they are prone to fracturing during these procedures. Broken IUD fragments can cause internal injuries, requiring additional surgery and potentially leading to long-term health problems.
According to TorHoerman Law, over 2,600 lawsuits have been filed against Teva Pharmaceuticals and CooperSurgical, the manufacturers of Paragard. The lawsuits argue that the manufacturers failed to adequately warn about this potential complication.
The first trial to test these claims is scheduled for October 2024. Its outcome could significantly impact future litigation and potentially influence broader conversations about IUD safety.
Frequently Asked Questions
Is reversible contraception safe?
Reversible contraception, including methods like LARCs, is generally considered safe and effective for most individuals. However, like all medical interventions, there are potential risks and side effects that should be discussed with a healthcare provider.
What is the 100% safest method of contraception?
Abstinence is considered the 100% safest method of contraception because it completely avoids the risk of unintended pregnancy and STIs. It involves refraining from any sexual activity that could lead to sperm reaching the egg.
Which contraceptive method is most suitable for an unmarried girl?
The best contraceptive option for unmarried girls will depend on personal preferences, health considerations, and lifestyle. Options like birth control pills or condoms provide effective pregnancy prevention with varying levels of convenience. LARCs such as IUDs or implants offer extended duration of protection and require less frequent maintenance.
In conclusion, LARCs have emerged as a game-changer in the world of birth control. From reduced cancer risk and regulated menstrual cycles to decreased PID risk and unparalleled convenience, LARCs offer a unique combination of advantages.
The Paragard lawsuit highlights the importance of discussing potential complications with your healthcare provider. However, it’s crucial to remember that LARCs are generally safe and well-tolerated.